Cavitation Surgery: an Exposé
Why did I elect to do a painful, expensive surgery that nobody seems to really care about?
A few reasons:
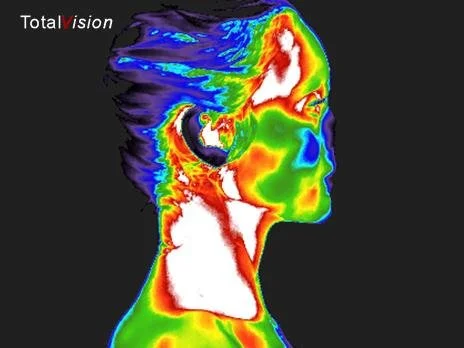
Inflammatory patterns persist on my right cheek/jaw in thermal imaging despite efforts to remediate.
Conebeam CT scan confirmed hole in the bones of all four of my wisdom teeth extraction sites by my biological dentist.
Emotional work regarding the certain issues in my personal life and how they correlate with the tooth meridian chart.
To attempt to relieve the burden on my immune system placed by these hole which harbor God-knows-what.
I’m in the mood to shed things that are not serving me. Letting go, let’s call it.
That’s a lot to dive into at once, so let’s just roll with numbers 1, 2, and 4.
I spent several weeks preparing for this surgery mentally and physically. The physical part involved supplements that supported bone growth and immune function, as well as addressing structural issues such as the upper cervical area of the spine, lymphatic drainage, soft tissue work, self massage, and chiropractic care. Mentally, I spent time in the quiet talking to my body about what I was allowing to happen to it (surgery), and that it should be prepared to receive this surgery as a pathway to peace (ultimately). It was important for me to make sure my nervous system wasn’t blindsided when the dentist would begin hacking into my gums and injecting chemicals to make me go numb when I arrived for surgery. My body and I were on the same page.
Top image indicates the cavitation encapsulated by scar tissue, which closes the area off from the rest of the body as a protective measure. This is the extraction site of Tooth 1 (upper right, back).
The process was actually grueling, and I consider myself pretty tough. I labored naturally with no medication for 42 hours (two of which spent pushing and knocking on death’s door) before an emergency c-section. This oral procedure might have been a little more trying on my nerves than the labor experience. I was awake for this procedure, but the site was locally anesthetized. It took four huge shots to numb the areas of the top and bottom third molar extraction sites on my right side. The numbness seeped throughout the intraoral tissue on the right side: I could feel it creep across the roof of my mouth and pervade down through my chin.
After confirming some things for me on my cone beam images (which were used to confirm the cavitations six months ago), like the severity of the situation and the nerve damage risk associated with surgery, I felt comfortable to lay back and let my dentist dig into the back of my mouth with one of his many prodding, sharp tools (unsure of exactly which tool, because I closed my eyes 🫣). Straightaway, he began hacking through gum tissue searching for a spot on the bone cap - the only bone that did grow back after wisdom teeth, a thin layer across the topthat he could penetrate. This would give him access to the holes left in my jaw where teeth once were all those years ago - these holes are what are known as a “cavitations.”
This was hard to sit through because I was aware of the force he was using to break through the bone in the back of my mouth - not that I could actually feel the pain, but I felt him wrestling with it and my head went back and forth with his hands as he forged his way through. He got to a point where he decided to use an electric drill instead of a manual tool because it wasn’t getting the job done, and that kicked out the smell of ground bone, another visceral part of the whole experience. The smell of bone and old, unhealthy tissue and blood were not things that any of the local anesthesia desensitized. Nope - I could 100% smell, and although I wasn’t feeling the incisions and drilling, I was definitely smelling it and that seemed to add a level of “real” to the process.
I have to admit that in retrospect, I appreciate not having gone fully under for this surgery. Lucky enough to find a kind and mild-mannered biological dentist, he was willing to explain the things in real time as he was navigating the whole procedure. I truly feel like that helped my nervous system accept the process much more than it would have if I had been unconscious. I almost felt like I got to be a parent to the child version of me, holding her hand through the pain, knowing on the outside that everything is okay, while maybe on the inside she was screaming and scared because someone was cutting and drilling into her. To this point, I’m glad we opted for local anesthesia instead of going fully under.
He started with the top cavitation: found the hole through a bone cap and some scarred tissue that had begun to wall off the cavitation in an attempt to protect my body from it. By walling it off, like your body does when you get a splinter, it is prevented from access to blood supply. Once he was in, he inserted ozone treatment to clean the bacteria and encourage angiogenesis - the growth of new blood vessels in an area. Blood brings nutrients and oxygen to the area, which is how it heals and regrows. He mentioned that there was no blood when he cut into it initially, and that to get bleeding he had to utilize the ozone. After it sat in the cavitation for a few minutes, blood started to arrive.
10 cc of my blood which has been centrifuged to separate fibrin from plasma. The fibrin is platelet-rich (known as Platelet Rich Fibrin, or PRF), and is implemented into the cavitation to stimulate bone regrowth and faster healing.
The ozone was step one when entry had been gained; step two was injecting platelet-rich fibrin, which was manufactured in-house by taking 40cc of my very own blood and putting it into a centrifuge to separate the plasma from the gooey fibrin in the blood. This fibrous goo, known as platelet-rich fibrin, or PRF in the medical field, can be used to stimulate bone growth and healing. It’s a relatively new technology that aids in cutting recovery time and expediting tissue growth.
After the ozone and PRF were administered, I was sewn up with a suture and ready for the same process on the lower cavitation.
Cut, drill, find hole, implement ozone therapy, insert PRF, seal with suture.
The whole process took about 90 minutes.
During the numbing stage at the very beginning, I could feel my nerves starting to act up. Of course they were - I was allowing my body to be cut into; I voluntarily laid my flesh on a dentist’s butcher board. My body was preparing to defend itself. To combat this, I tried to gain presence and talk to myself like the parent of a child: “we practiced this, and we have given our permission for this to happen. This is completely expected and welcomed because it’s going to help heal us on a deep level, and we want the benefits of this procedure. Use your mind to welcome this and take a deep breath.” This language helped me navigate the whole experience while being able to consider the impact it was having on my nervous system.
I also used some breathing techniques I’ve been reading about in the book Breath by James Nestor, remembering the importance of breathing out fully, making myself aware in the operating chair of my exhales and doing so for twice as long as an inhale. This increases CO2 in the blood and allows the body to retain and utilize more oxygen. I paired this with some Heart 7 point acupressure on both wrists to try to keep any manageable anxiety at bay.
The scope of red light therapy is vast and almost even unknown. I immediately implemented red light exposure to the surgical site (exterior) immediately post procedure.
After those 90 minutes were over, I was sore and swollen and exhausted from the madness I had just subjected myself to. I was grateful for the opportunity, but needed to get home and rest to recover from the trauma. At home I had homeopathic pain pellets, a warm bed, and lots of charged up red light devices ready to get to work. Admittedly, I had the best nap after that, but when I woke up, the local anesthesia had worn off completely, and I was introduced to the true extent of the pain, which was waiting for me post-surgery. Wow.
I can describe the pain as somewhat of an amped up version of strep throat mixed with taking a hook shot to the jaw: it feels like the back of my throat is very inflamed and it’s especially noticeable when I swallow. It’s warm back there, extremely sore, and sensitive to the touch (from the outside) from my chin through to my ear. There’s a heavy pressure bearing down on the whole back right quadrant of the oral cavity. It’s pretty significant.
The pain was the worst from hours 5-10 following the surgery. I also noticed bleeding until about 8 hours afterward, though not a ton. I could taste it. I was unable to attempt even a sip of water until 12 hours had passed. I had some luck with warm beef bone broth, added turmeric, salt, and ghee, and found that it might have actually made me feel a little less sore. I also had some green juice and realized my body was craving nutrition - this surgery was at 7 am, so I had been going on almost 24 hours of intaking no nutrition. I ended up downing 32 oz of beef bone broth and then half a can of split pea soup, along with about 8 oz of green juice around 11 hours post-surgery.
Sleeping that night wasn’t as bad as I thought it would be. I didn’t take any pain meds, either. Since brushing wasn’t an option, I lightly rinsed with warm water (without spitting or sucking), and then applied Oral Supreme on the gum lines opposite side of the incisions. One yucky reality about this situation: my mouth feels so gross. The taste of blood and the inability to swallow comfortably - I feel very unclean inside my mouth, and I’m the kind of person whose oral hygiene determines her comfort zone, and this ain’t it.
Living on nutrient-dense, high calorie liquids is the fastest, safest, and most effective way to recover from any intraoral surgery. Turmeric has powerful anti-inflammatory properties.
One measure I was sure of before bed was to implement the mouth tape. The last thing I need in the healing process is to offer a gaping mouth to the wound, increasing bacteria proliferation and interrupting the healing process with dry, unwarmed mouth air. It needs to stay moist and the mouth needs to stay shut. I noticed in my nap after the procedure that my mouth was tending to open a little due to the swelling - the tape solved that overnight.
I slept pretty well despite the pain. I made sure to keep myself semi-propped up, as I was advised to do at my appointment. My sleepy-time cocktail served my needs well; I usually do a combination of magnesium, Albizia Supreme, and a serotonin support supplement called Travacor to ensure sleep when I feel like it might not be so easy. This night, I slept.
Waking up reminded me of the pain I was in, and it was not much better. It was more achy than acute, and definitely still big. And the throat part was really sore; it hurt each time I swallowed. I didn’t feel comfortable trying to open my mouth very big, or even at all. On top of the pain, it was also very icky in there when I woke up. I am really looking forward to be able to get some good swish and brush action.
The reason I can’t swish or spit right now is to protect the clotting process. If you knock a new clot loose, you run the risk of a dry socket or infected site. Swishing, sucking through a straw, spitting, or blowing the nose can cause loss of the blood clot, which can lead to more bleeding (obviously) and a dry socket. Starting 24 hours after the surgery, it should be safe to start gently swishing with warm salt water.
And since the surgery, it’s been bothersome to have to talk. I almost feel like it’s going to cause bleeding if I have talk too much. I don’t even want to have to open my mouth big enough to put a spoon of soup into it, much less open it big enough to form words intelligibly. Paired with what feels like strep throat on one side, talking is something I’m taking a break from unless I have to.
There’s significant swelling, limited to the right side of my face and very noticeable when I try to smile. Some people experience bruising with this procedure, but I don’t notice any. Keeping my red light on the swelling, but not treating with ice packs or heat packs so as not to manipulate the inflammation - it was called to this area to heal this area, and I’m not going to do anything to send it away sooner than it needs to.
Truthfully, I have forgotten the size and nature of oral surgery since that wisdom extraction nearly two decades ago. It’s big. The OTC pain meds have tempted me a few times in the past 36 hours (but were denied). I was honestly hoping to roll out of bed the next day and go about life, but it’s a sobering reminder of the seriousness of what just happened - you have to give the body what it needs to heal, which is time and care. I’m learning patience through this one.
I’m bent on making sure this remediation has every chance to fulfill its potential. The important part of healing seems to be taking care of the incision in the days that immediately follow the surgery - that is, allowing the area to clot properly and not have to combat added stress of things like sugar which would feed bacterial infections and increase the risk of developing infections, foods you have to chew that can become lodged in the area, and the pressure of typical mouth activity like straw use (which can dislodge an early clot), nose-blowing, or even swishing with water and spitting. These careful measures will go a long way in the ultimate healing progress; making sure those first 48 hours are dialed in are, in my opinion, the most important part of the whole experience, because everything hangs in that specific balance.
Supplements I’ve utilized to prepare pre- and post-surgery:
Lu Rong Supreme
Bone And Marrow (Ancestral Supplements)
Manjistha Supreme
Oral Supreme
Reishi Supreme
Camu Supreme
Takesumi Supreme (binder - no idea what was released from surgery site)
Liposomal Glutathione (Quicksilver)
Liposomal Vitamin C (DesBio)
Ozonated Oil Pulling Solution (PurO3)
D3 + K2 drops (Thorne)
SBO Probiotics Trinity (Ancient Nutrition)
HCl + Betaine (Thorne)
Trace Minerals (Pure Encapsulations)
PC liquid (BodyBio)
Collagen (Orthomolecular)
Liquid Chlorophyll (NOW)
StellaLife Recovery kit (spray, rinse, + gel)
Arnica Montana 30 c
Staphysagria 30 c
Horsetail tincture
Nettle Leaf Tea
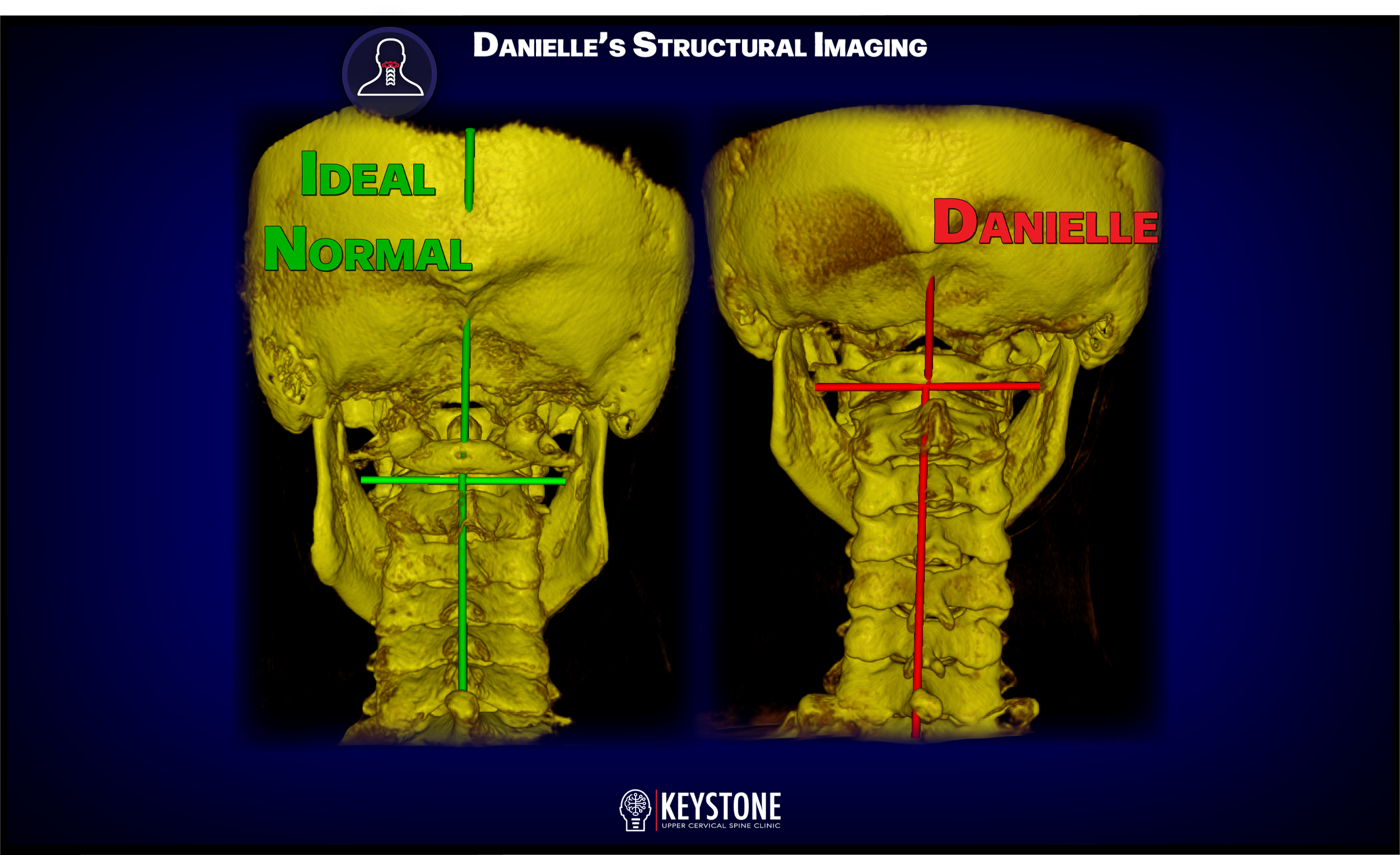
Upper cervical evaluation provided new clarification that might suggest blood flow restriction to the right jaw, as well as insight into nervous system patterns and their influence on physiology.
Further considerations for prepping pre- and post-surgery:
Lymphatic therapy sessions twice monthly for 3 months using LymphStarPro on jaw and neck
Upper cervical adjustment tailored to me, and soft tissue work around the UC area
Cupping on the upper back to release the shoulders from the neck and promote spinal health
Self-massage of the jaw area tissue, the SCM, the ears, and the medial pterygoid inside the mouth
Diet rich with collagen and protein and other bone-building components (absent of sugar)
Meditations that involved accepting surgery; positive inner dialogue around the procedure
Interviewed several qualified professionals about the process, their experience, best ways to prepare the body, the necessity of surgery, etc. My approach was ask too many questions and have too many answers instead of asking no questions and having no answers. That gave me confidence to move forward.
Cavitations outside of my personal experience
Living with cavitations is dangerous for many reasons. The first, most obvious reason is that they can be breeding grounds for inflammation and infection: they are dark, moist holes in the back of the throat that have priority access to all the foods, sugars, viruses, and bacteria that enter through the mouth. Things like that get in there and then “get cozy,” meaning they choose to build biofilms or other protective barriers around themselves to ensure that they remain fed and housed, and not evicted by all the herbs and supplements we take to combat them.
Cavitations place burden on the immune system because they demand extra from it, requiring more metabolic attention, more nutrients from blood supply, sympathetic nervous response, and ongoing healing. This in turn results in lowered immune function, overworked lymphatic nodes (think of allllll those lymph nodes right near the jaw on the neck), and can possibly explain those elevated WBC counts in blood work that never seem to budge.
Just to give you an idea of what’s possible, look at my experience: there were bone fragments hanging down in a dead hole in my upper jaw, like stalactites in a cave, with no blood supply, surrounded by scar tissue to keep it segregated from the functioning whole of my body. And in the bottom jaw was found a fatty oil cyst, which, in an area only 1.5 centimeters cubed, is alarming because it doesn’t leave a lot of wiggle room. Two completely varied outcomes in areas of the same person from the same surgery on the same day. Imagine what’s possible. I can fathom that the cyst might have continued to grow, especially since it actually was getting blood supply, unlike the stalactites in the dead hole of the upper jaw. That cyst could have continued growth, harbored disease, and resulted in a plethora of unexplained immune responses (including not being able to tame the hardened lymph nodes in my neck).
Thermal image indicates inflammation on the area of the right jaw, possibly due to cavitation (which was later confirmed by ConeBeam CT).
Cavitations aren’t talked about much at all in mainstream alternative health (how’s that for an oxymoron?), or at least not yet. Hopefully I can help forge the path for people, who like me, took the advice of their traditional dentists as a young adult and underwent surgery to remove their wisdom teeth, with no warning whatsoever that the bone would likely not regrow to fill in the now empty holes in the jaw. And not just without warning, but also without explanation. It seems almost criminal to put people in these situations, now knowing the extent of cavitations. The data has arrived. The test group (us) has been analyzed: 85% of wisdom teeth extractions result in cavitations. THAT’S PRETTY MUCH ALL OF US WHO HAD WISDOM TEETH REMOVED. This, in my opinion, has the potential of being a sleeping epidemic - once we open the lid on this, it could solve so many people’s issues.
Final note:
It’s expensive, and it’s not covered by insurance. In full transparency, I paid $6800 for this (remediation of 2 of the 4 cavitations). Check with your dental insurance companies, bug them about covering it. It’s more than warranted and it’s not covered. This is a position dentists have been putting people in for decades now, and they’re leaving folks out to dry with an enormous bill when they’ve washed their hands of the damage they caused years ago.
I’d love to hear your experiences with wisdom teeth removal (also known as “third molar extractions”), Cone Beam CT scans, cavitation remediation surgeries, jaw infections or inflammation, thermal imaging of the head, or anything else that could possibly be related to this widespread issue. I’d also love to know if this is all brand new to you, and if you have any concerns yourself. Remember - you can always image with thermography to get an idea of the inflammation in your face. And I can help you find thermographs in your area - find me on Instagram and send me a message. Please drop all your thoughts in the comments. Let’s work together to bring understanding to this important issue!